Adolescent Idiopathic Scoliosis
Non-Operative Scoliosis Treatment
The majority of individuals with adolescent idiopathic scoliosis (AIS) do not need surgery but rather are observed (monitored over time) or braced. Small curves below twenty degrees or curvatures up to 40 degrees in skeletally mature patients do not require surgery or bracing. If curves progress in the still growing adolescent, bracing is recommended for curvatures between 25-40 degrees. Patients are closely followed and evaluated at 3-6 month intervals typically until skeletal maturity. Once growth has ceased, evaluations are less frequent.
Observation
Observation is an active form of treatment in which the patient is closely monitored for signs of worsening (progression) of curvature. If progression is noted, bracing or surgery may be required. Patients are monitored by physical examination and usually x-rays. Patients are offered Scoliscan (Diers Formetrics) light-based surface topography so that they can be followed over time without x-ray. If a change in the body surface measurements is noted, xrays, the gold standard, are performed and treatment recommendations are made.
Bracing
Bracing is indicated for curvature of 30-45 degrees in a growing adolescent or progressive curvatures between 20-30 degrees. Bracing has been shown to be effective in decreasing curve progression to a surgical range or to 50 degrees or more compared to observation alone in a prospective randomized controlled trial (the highest level of clinical proof or evidence in medical research). In this study, the BRAIST study, the amount of time the patient spent in the brace was found to be important in preventing curve progression. From this, we and others recommend brace wear of between 16-20 hours for most patients.
There are numerous types of braces and proponents claim the brace they use to be the “best” brace. The most important aspect of bracing is that the brace is well-fitted and that the patient is compliant with bracing, that is they wear the brace for the prescribed number of hours per day. The brace must provide a correction of the curve approaching 50% when the patient is in the brace in order to be effective. This does not imply that correction at the end of bracing will be 50% but rather that a good corrective force is being applied. Brace success is defined by the main curve not progressing.
Does Bracing Work to Prevent Scoliosis Progression? The BRAIST Study
In 2013, the Bracing in Adolescent Idiopathic Scoliosis Trial (BRAIST) study was published in the New England Journal of Medicine. This study was significant in determining the effectiveness of bracing, as compared with observation, in prevention of curve progression to 50 degrees or a recommendation for surgery.
Twenty five institutions throughout the US and Canada collected data on 242 patients who had curves for which bracing was indicated (20-40 degrees). The participants were aged 10-15 years old, and had Risser scores of 0-2 (indicating growth was not yet complete). One hundred forty six patients wore braces for the study, while 96 were observed only for curve progression.
Patients who wore braces used the thoracolumbosacral orthotic type most commonly utilized in their institution’s clinical practice; most wore Boston style braces. They were instructed to wear their braces for a minimum of 18 hours/day, and a temperature logging tool within the brace confirmed compliance with these instructions. Patients were evaluated, including x-ray, every 6 months during the study.
Bracing success was defined as reaching skeletal maturity (the end of growth) without progression to a 50 degree curve. Failure was defined as curve progression to 50 degrees and/or recommendation for surgery. Seventy-two percent of patients who wore a brace were considered successful, while only 48% of patients who were observed without wearing a brace had a successful outcome.
Additionally, the amount of time the patient wore a brace correlated with the rate of success. Patients who wore their brace for 0-6 hours per day had only 41% success. This was similar to the results of those who were observed without wearing a brace. Meanwhile, those who wore their braces for 18 hours per day, as instructed, had a success rate of 90-93%.
The BrAIST study provides strong support for the conclusion that bracing reduces the risk of curve progression and need for surgery. It also shows the importance of wearing a brace for the prescribed number of hours per day. You can read the study itself at http://www.nejm.org/doi/full/10.1056/NEJMoa1307337.
“In adolescents with idiopathic scoliosis who were considered to be at high risk for curve progression that would eventually warrant surgery, bracing was associated with a significantly greater likelihood of reaching skeletal maturity with a curve of less than 50 degrees, as compared with observation alone.”
Patient Story 1:
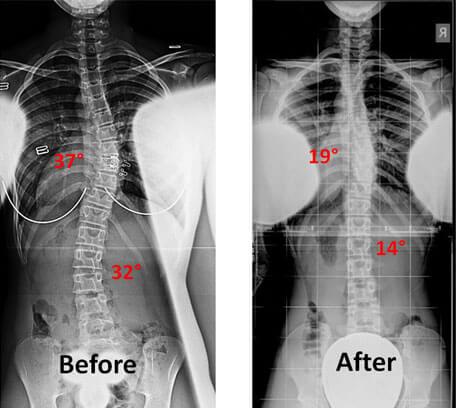
Niara came to see us when she was 11 years and 10 months old. She had a right thoracic curve of 33° and a left lumbar curve of 30°. She also had a strong family history of scoliosis with her brother undergoing observation for curve progression, and a cousin undergoing surgery to correct her scoliosis. Niara, who is a fashion model, wore a low-profile brace for 4 years and has done remarkably since. She writes, “I now stand at 5'8.5 still growing, more than 20 fashion shows in New York city, modeling for 2 major hair companies, yet more to come and still in school maintaining an 85 grade point average and better.” Read more about her story here. (link the word here to testimonial page where Cathy’s story can be found) Show Niaras x-rays before and after surgery along with one of her modeling pictures.
Patient Story 2:
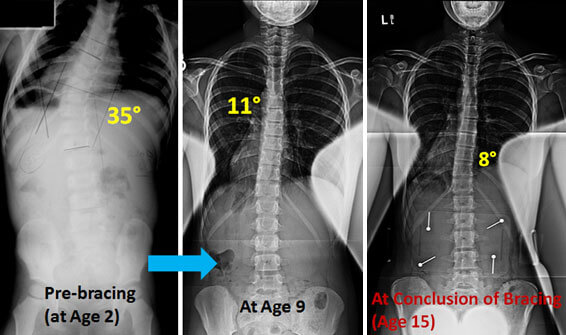
Brielle is now 15 years old. She was diagnosed with infantile idiopathic scoliosis and had a left thoracic curvature of 35° at 18 months of age. Brielle started to wear a brace when she was 2 years old. Her thoracic curve was reduced from 35° to 12° after just 2 years of a full time bracing program. Her curve has been stable since then and was maintained during her pubertal grow spurt. Her brace wearing time was gradually decreased from 20 to 12 hours/day. Brielle is very active and plays competitive basketball. During her most recent visit, her curve was stable at 9° with her being out of the brace for three days prior to the visit. Brielle has been out of her brace for over a year now. She has been a stellar patient who was committed to her bracing regimen over many years along with the love and support of her family.
Brielle’s case is a dramatic example of the benefits of bracing as recently emphasized by the publication in the New England Journal of Medicine of the prospective, randomized, multicenter, NIH-funded BRAIST study in adolescents undergoing bracing.
Scoliosis-Specific Exercise Therapy
There has been a movement in recent years toward the use of specific exercise and physical therapy programs directed toward the treatment of scoliosis. Although the highest level of clinical evidence is still lacking for these techniques, we do believe that exercise and physical activity in many forms are useful in helping patients with postural realignment, decreasing muscle fatigue and discomfort, and improving breathing mechanics. To date, little evidence exists that curve progression can actually be stopped with exercise and/or physical therapy methods alone, but clinical trials are ongoing that hope to answer this question.
The Schroth Method
The Schroth Method is a physical therapy technique developed in the 1920s specifically for scoliosis. Its thesis states, “scoliosis involves asymmetrical muscle groups in the back and elsewhere, which in normal bodies are more evenly symmetrical.” The method, therefore, consists of exercises meant to strengthen certain muscles around the spine and within the torso while stretching and lengthening others. Its goals are to reverse abnormal curvatures and associated pain.
Schroth Method exercises are coordinated in three dimensions, sagittal (side to side), frontal (front to back), and transverse (top to bottom). They include breathing techniques, pelvic corrections, isometric contractions, and posture practices. Therapy is tailored to the individual. The aim is to teach the patient about his or her own body, and demonstrate practices that can be implemented in daily life rather than just during exercise sessions. We have certified Schroth therapists available at our Manhattan location who can be contacted for an appointment.
Physical Activity
While physical activity and formal exercise are important in everyone’s daily life, exercise is especially important for patients who wear a brace and have scoliosis and/or kyphosis. Exercise strengthens the muscles of the back and abdomen (the so-called core), thereby decreasing episodes of back pain throughout your life.
• Yoga and Pilates are great ways to stretch and strengthen your back. They improve core strength, which supports the spine and assists in posture. Practice either to your comfort level. In many cases, informing the instructor that you have scoliosis will prompt him or her to offer variations of the postures. Additionally, we have resources in our office for scoliosis-specific yoga instruction.
• Swimming is an exception to out of brace time for up to 4 hours.
• The doctor may instruct additional exercises or individualized therapy to compliment your brace wearing regimen.
Surgery
Surgery is recommended for curves that progress beyond 40 degrees in the growing child or more in the skeletally mature adolescent. For large progressive curvatures, delaying surgery typically results in worsening of the curvature and may change the type of surgical procedure that is recommended and make it more extensive such as requiring more levels of the spine to be fused. Therefore, it is important for the family to be well informed of treatment options and to agree on a plan with their treating physician which can be modified over time as necessary.
The goals of surgery for AIS are to correct spinal curvatures, to maintain as much motion and flexibility of the spine as possible, to prevent the sequelae (results) of untreated scoliosis later in life such as back pain, difficulty breathing (pulmonary problems), neurological deficits (numbness, weakness), disability and disfigurement. There are numerous surgical options available depending on the severity, location of the curve, and the age and growth potential of the patient. The option recommended by the surgeon is designed to achieve three dimensional correction of the spinal curvatures with the least risk and the easiest recovery possible. Below are a number of procedures and approaches that are performed by Dr. Lonner and his team.
Posterior Spinal Fusion with pedicle screw instrumentation
Corrective surgery for scoliosis most commonly involves a fusion or biological welding of the segments of the spine [see spine fusion]. This is now most often performed from a posterior (back) approach in which all structural curves of the spine are fused. Structural curves are large, relatively stiff, and are associated with body shape spinal curvatures. The posterior surgery today is performed with rods and pedicle screws. The screws provide a very powerful anchor to the spine which makes corrections better than in past eras of surgery (15 years ago) and loosening of implants much less common than previously. In the past, more anterior (front) techniques were performed but this is now reserved for only select cases [see VATS]. AIS can occur as a single, double,or triple curve and may be located in the thoracic (ribbed) spine or the lumbar (lower, non-ribbed) spine. Below are examples of patients with single, double or triple curves treated with posterior surgery. In the past, even small curves in the lumbar spine were fused as part of the operation to correct a structural thoracic curve. This was thought to be a good approach because it resulted in excellent corrections of all curves. The downside is that it stiffened segments of the spine that did not have structural curves. Today, selective fusions are performed to only correct the structural spinal curvatures and maintain motion. Dr. Lonner has been a co-investigator (researcher) in a multi-center study nationwide studying motion in the unfused lumbar spine following surgery out to 10 years. The good news is that in the AIS patient, even with fusions into the middle of the lumbar spine (L3), motion, and therefore, activity level is maintained!
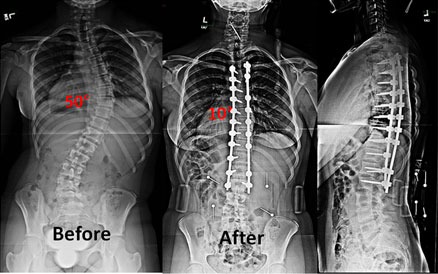
Single Curve
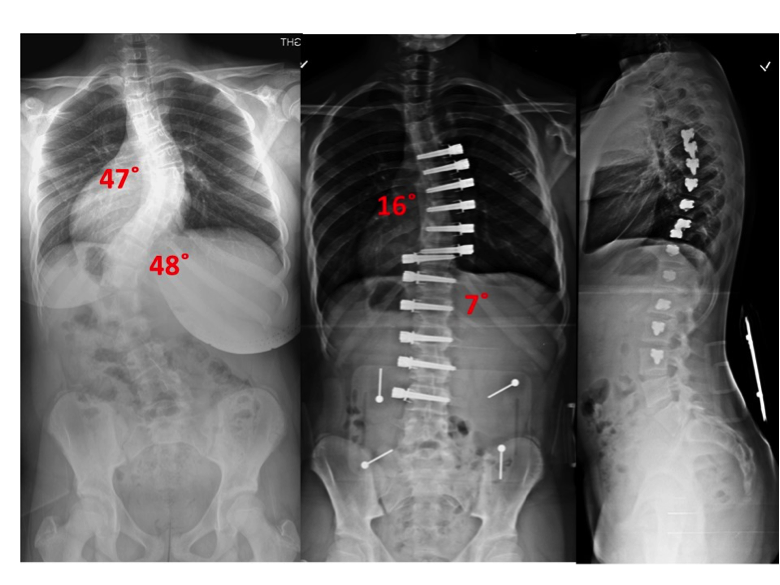
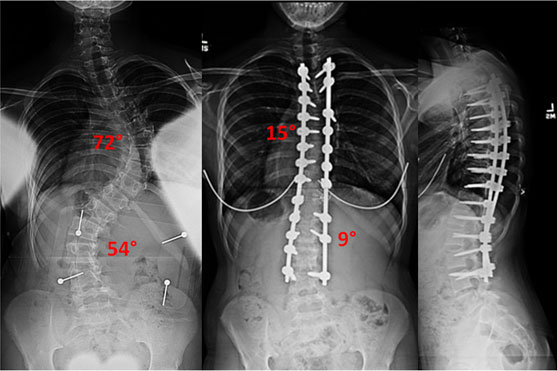
Double Curve


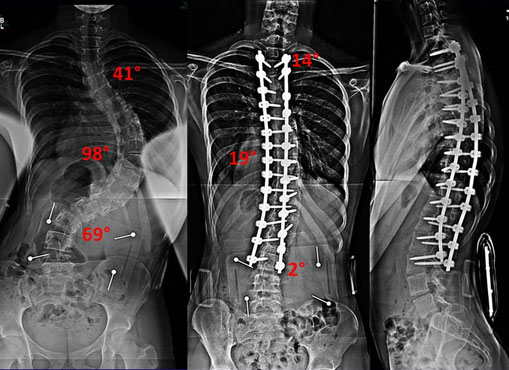
Triple Curve

Large Curves

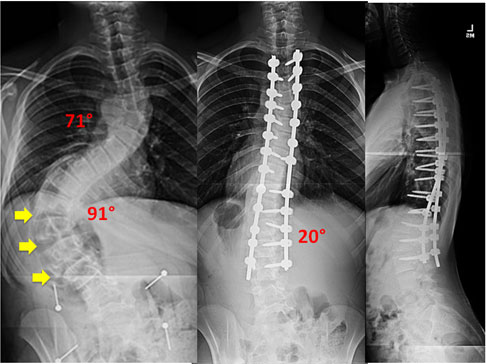
Although most curvatures are not severe, some patients have very large curvature with severe spinal curvatures. This is an area of expertise of Dr. Lonner. The large curves often require more advanced surgical techniques to be optimally corrected. This includes performing anterior (front) surgery with minimally invasive techniques [see VATS] or from a posterior approach. Dr. Lonner is an international leader in the development of these approaches which only a handful of surgeons around the world have expertise in. For other patients, various osteotomies (cutting into bone to make the spine more flexible) are used to get the best
correction possible. These osteotomies require a surgeon with vast experience to be performed safely.

This patient underwent a combined VATS procedure with posterior spinal fusion to correct this severe progressive scoliosis.

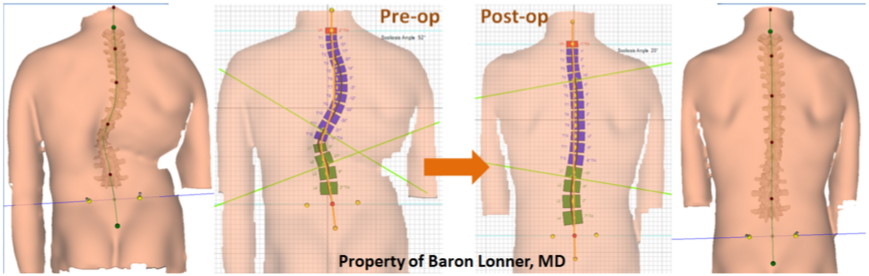
This patient had a new approach, that Dr. Lonner developed, to correct severe curvature by removing several discs from the back of the spine to make it more flexible to allow maximum correction. The Scoliscan surface topography shows the dramatic changes in the patient’s body shape from before to after surgery.
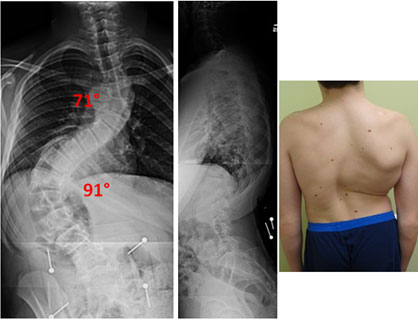

Osteotomies are a means to correct severe scoliosis by cutting into the bone and removing portions of the spinal column to achieve correction in the safest way possible. If the surgeon attempts to correct such a severe curvature as below without removing part of the spinal column (Vertebral column resection), the spinal cord can be stretched and the blood supply affected causing paralysis potentially. The patient below did very well and has a normal neurological examination after the surgery.
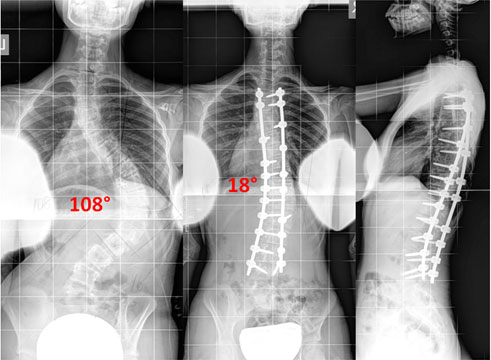
Pre Op


Fusion-less Surgery
Most surgery for AIS is done by fusing the spine and using solid rods and screws that correct the curvature but eliminate motion. The future (and present) of scoliosis surgery in growing children includes non-fusion approaches in which the patient’s remaining growth will be taken advantage of. Growth is guided to help gradually straighten the spine and spinal motion is preserved. This approach is called growth modulation, performed with either spinal stapling or spine tethering. Stapling is now rarely performed and is only effective for small curves. Dr. Lonner is one of only a few surgeons worldwide who performs these procedures which are still being developed and allow for continued growth, flexibility of the spine, and full activities without restriction. Learn more here.
This 12½-year old girl is an avid basketball player and horseback rider. She underwent vertebral body tethering procedure, which was performed by Dr. Lonner, with excellent correction of her scoliosis. She was allowed to return to full activities 6 weeks following surgery. The video shows the patient bending 3 weeks after surgery.
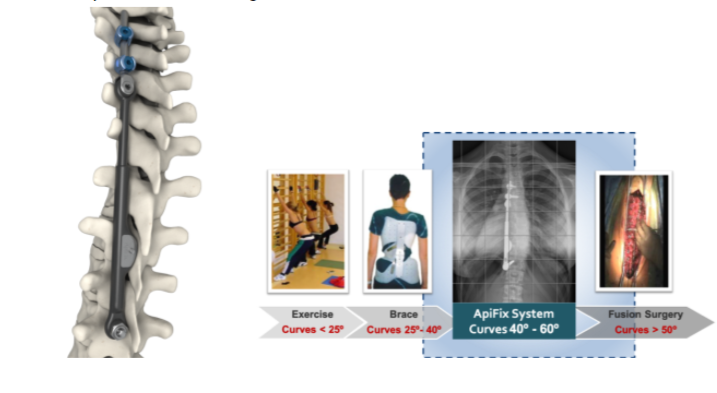
ApiFix
A new approach to non-fusion scoliosis correction is termed posterior dynamic scoliosis correction using the ApiFix device which was FDA-approved in the United States in September of 2019. This device has been available to treat patients with adolescent idiopathic scoliosis in Europe and Israel for the past nearly one decade. Dr. Lonner has consulted with the ApiFix company and was instrumental in dealing with the FDA to help to bring this option to patients in the United States.
ApiFix is placed in patients through a posterior (back) approach, and it allows for correction of the spine without fusing the entire length of the curve as occurs in spinal fusion. There is some overlap in indications for VBT and ASC. Dr. Lonner and his team will discuss which option may be best for you based on your own preferences and ideal indications. Ideal candidates for ApiFix are adolescent patients with curves between 35 and 60 degrees and only a single curve. There is minimal blood loss and return to activities within 3-4 weeks. Patients who have failed bracing or who are unable to comply with bracing may be the best candidates for this procedure especially if they have further growth remaining and are likely to experience worsening of their curvature. The device is shown below.