Dr. Lonner
A Family’s Journey: Seeking Support for Their Daughter’s Post-Surgery Recovery
In the heart of Buckeye, Arizona, the King family is facing a challenging journey that has captured the hearts of many. Their story is a poignant reminder of the strength, resilience, and love that binds families together, even in the face of overwhelming adversity.
A Life-Changing Diagnosis
For the King family, the year 2024 brought unexpected trials. Their daughter, who has shown incredible bravery, was diagnosed with a rare condition that required specialized surgery. This wasn’t a straightforward procedure that could be handled close to home. Instead, the family had to travel across the country to New York, where expert surgeons could perform the life-saving operation.
The surgery, while successful, was only the beginning of their battle. Recovery for such a procedure is complex, demanding, and full of uncertainties. It’s a time when being surrounded by loved ones and familiar environments can make all the difference in healing. But for the King family, the journey back home to Buckeye has become an uphill battle.
The Struggle to Return Home
After the surgery, the family found themselves stranded in New York, far from the comfort and familiarity of their Arizona home. The physical and emotional toll of the situation is immense. Imagine the stress of navigating a bustling city far from home, with a child recovering from major surgery, and the daunting task of figuring out how to get back home safely.
Financially, the trip has been overwhelming. Medical bills, travel expenses, and the cost of living in New York have drained the family’s resources. They have exhausted their savings, leaving them in a position where they must reach out for help.
A Community Rallies Together
This is where the power of community shines through. The Kings’ story has touched the hearts of many who are eager to help. Friends, neighbors, and even strangers are coming together to support the family during this difficult time. A GoFundMe campaign has been set up to help cover the costs of their travel back to Buckeye, as well as ongoing medical expenses.
The outpouring of support has been incredible. Donations, words of encouragement, and offers of assistance have flooded in, showing the King family that they are not alone in their journey. Each contribution, no matter how small, is a step closer to bringing them back home, where their daughter can continue her recovery surrounded by the love and care she needs.
How You Can Help
The King family’s story is a powerful reminder of the importance of community and compassion. In times of crisis, the support of others can be a beacon of hope. If you feel moved by their story, there are several ways you can help:
- Donate: Contributing to the family’s GoFundMe campaign will directly help them cover the costs of travel and medical expenses.
- Share: Spread the word about the King family’s situation. The more people who know, the more support they can receive.
- Offer Encouragement: Sometimes, a kind word can make all the difference. Leave a message of support for the family as they navigate this challenging time.
Conclusion
The King family’s journey is far from over, but with the continued support of their community, they are one step closer to bringing their daughter home. It’s in moments like these that we are reminded of the strength of the human spirit and the power of coming together to help those in need.
If you’d like to follow the King family’s progress or contribute to their cause, please visit their GoFundMe page. Every bit of support helps bring them closer to home.
Surgeon Paves the Way for Non-Fusion Correction of Scoliosis
https://reports.mountsinai.org/article/ortho2021-02-mount-sinai-surgeon-paves-the-way-for-non-fusion-correction-of
Mount Sinai orthopedic surgeon Baron S. Lonner, MD, is leading the charge to add vertebral body tethering to the spine surgeon’s toolbox. Dr. Lonner has performed more procedures using the device than any other surgeon worldwide.
In August 2019, vertebral body tethering (VBT) was approved by the U.S. Food and Drug Administration, joining spinal fusion and rigid bracing as time-tested options to treat adolescents with abnormal lateral or side curvature of the spine whose bones have not fully matured. The approval marked an exciting new era in corrective surgery for idiopathic scoliosis and Mount Sinai orthopedic surgeon Baron S. Lonner, MD, is leading the charge to add the procedure to the spine surgeon’s toolbox. Having performed nearly 350 VBT procedures in recent years—more than any other surgeon worldwide with the approved device—Dr. Lonner is well positioned to lead the pack.
Currently, two surgical non-fusion devices have been approved by regulators in the United States. The Tether™ Vertebral Body Tethering System, which was developed by Dr. Lonner and other surgeons as well as a group of engineers, and the ApiFix System (ApiFix Ltd., Israel) for motion-sparing scoliosis correction. Dr. Lonner played an advisory role in the latter device.

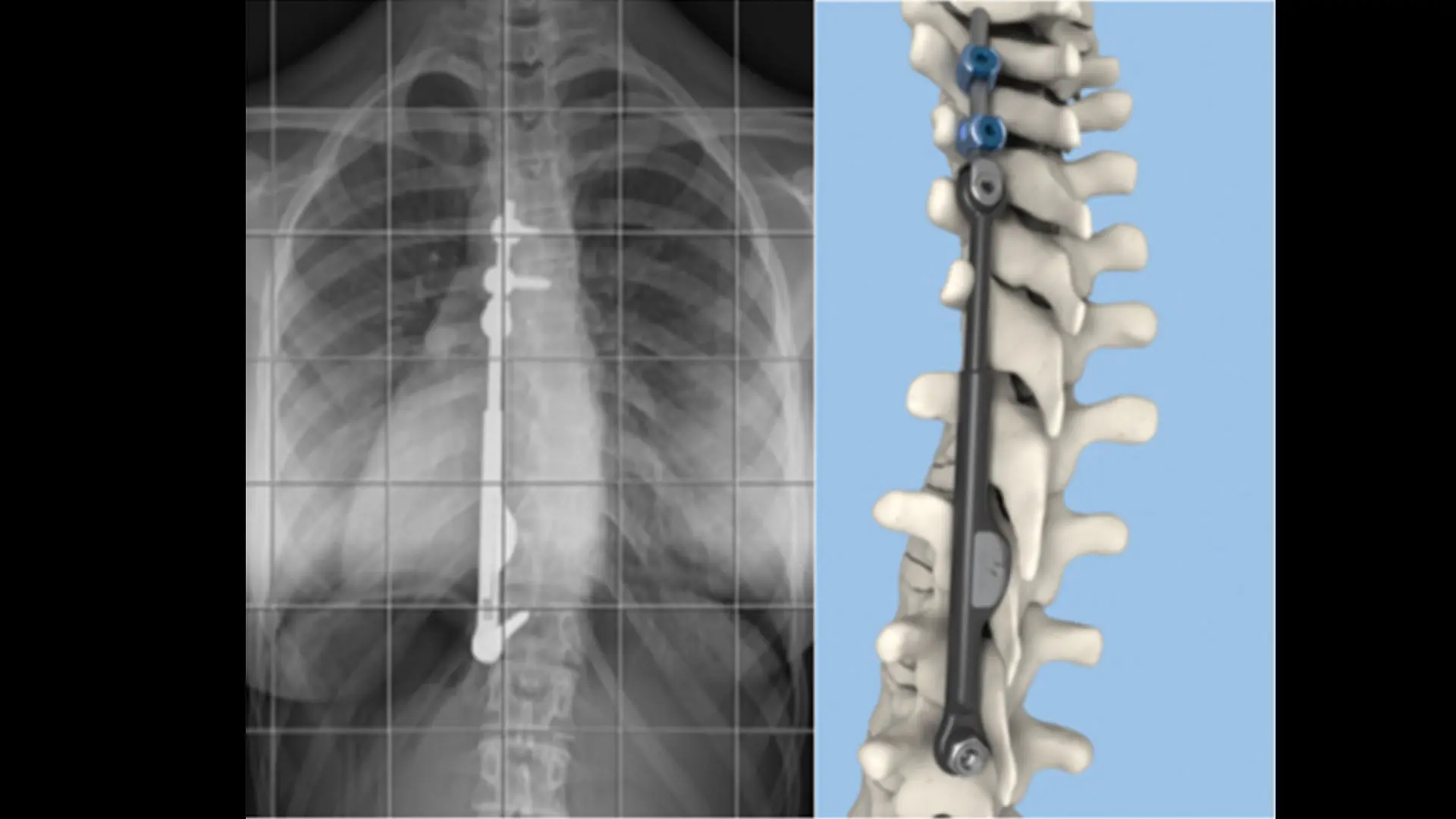
“Spinal fusion has performed well traditionally for people with severe spinal deformity, and remains the gold standard,” says Dr. Lonner, who is Chief of Minimally Invasive Scoliosis Surgery and Professor of Orthopedics, and Pediatrics at the Icahn School of Medicine at Mount Sinai. “But if the curvature is moderate and more flexible, then the Tether can deliver excellent outcomes. In fact, we have seen correction of a 50-degree curve down to about 15 degrees or less, for example, while preserving spinal flexibility and function over time. And, patients are able to return to sports and other activities soon after surgery.”
Surgical Differences in the Approved Devices
Dr. Lonner continues to work with industry partners and their engineering and manufacturing arms to nurture the next generation of high-performance, non-fusion technologies and devices for spinal correction. For now, Tether and ApiFix are underscoring the surgical possibilities.
During the Tether procedure, the surgeon places an anchor and bone screws made of a titanium alloy into the patient’s spine on the convex (outwardly curved) side of the spinal curve through an anterior approach. With the help of thoracoscopic visualization and very small incisions, a flexible cord made of a polyethylene-terephthalate polymer is secured to the bone screws, and the surgeon applies tension to the cord to partially straighten the spine. After surgery, the cord continues to straighten the spine while the patient grows.
The ApiFix System is somewhat different, attaching to the spine on the concave side of the curve and maintaining a good deal of the patient’s natural flexibility through a self-adjusting rod mechanism that allows for additional post-operative correction. This procedure is performed from a posterior or back approach. The device can even be removed if the curve remains straight after a corrective period of three or more years. “ApiFix works well for children who have failed with an external brace—either their curve is getting worse or they cannot tolerate it emotionally or psychologically,” notes Dr. Lonner.
The Path Ahead for VBT
Dr. Lonner acknowledges there is a steep learning curve for vertebral body tethering, which might detract from quick and widespread adoption by the orthopedic field. Nonetheless, he has seen a good deal of enthusiasm among colleagues around the world for the now-approved technology, as evidenced by the numbers of surgeons undergoing training to become certified in the use of the technique for their patients. “There will always be a role for fusion surgery because of its ability to address larger curves,” Dr. Lonner allows, “but VBT and ApiFix have shown they can produce dramatic corrections in children with remaining growth. Just as importantly, having these tools available will allow surgeons, together with patients and their families, to be more proactive in addressing spinal curvature earlier on—before it becomes severe and requires fusion correction.”
Concludes Dr. Lonner, “Given the various options I can now offer my patients, this is a truly inspiring time to be a spine surgeon.”
Featured

Baron S. Lonner, MD
Professor Orthopedic Surgery and Pediatrics
Keegan undergoes VBT
Thrown For A Curve – full from Sheryl Matthys on Vimeo.
Source – https://keegancares.com/scoliosis/
For years I’ve taken dance classes, gymnastics, and performed in musicals. Because of my activities, I thought my back was ‘tight’. I’ve been to the doctor for colds, concussions, and other things, but we didn’t know to ask ‘to get checked’ for scoliosis.
My diagnosis went unnoticed until one day at the age of 13 while at Wittler Orthodontics, the office manager Julie Downs spotted my shoulder blade sticking out. She called my mom later that day after talking to her boss as to whether she should say something. We’re so grateful she spoke up.
Upon consulting with several doctors in various states, my diagnosis of a 48º curve was too late for bracing to be effective. My best option was surgery. I underwent VBT (vertebral body tethering of T5-T12) which is a newly FDA approved surgery that uses a rope to maintain spine flexibility instead of fusion with two steel rods.
In my state, our legislature decided scoliosis screening was not necessary for schools and that pediatricians could handle it.
I’m an example that doesn’t work.
Had my school screened for scoliosis, had my doctor done the Adams Forward Bend test or used a scoliometer at any of my ‘sick’ visits, it may have been caught sooner. Doctors may only screen on a designated ‘wellness’ visit or possibly at a sports physical.
This leaves too many kids left unchecked.
And, it’s such a fast and simple thing to do.
It’s my mission to speak with schools and youth groups of the signs of scoliosis and to have schools annually check kids grades 5 to 8 via the Adams Forward Bend Test. I share my ‘before’ photo as a flyer so you can spot the signs of scoliosis too.
I have a speech, a talk, and flyers. Contact me if you’d like the flyer on the right sent to you and/or to speak to your organization or if you’d like to support this not-for-profit cause.
Keegan Cares, Inc is a 501(c)(3) organization.
COVID-19 Update May 2020
Dear Patients and Your Families,
Finally, we are getting the team back together after we have been separated in order to be mobilized to care for patients in the fight against COVID-19. My team and I will be proceeding with patient care. We have been doing many Telemedicine visits with pre-operative and post-operative patients as well as for non-surgical patients. We will start seeing patients in the practice on May 19th. Our first surgery will be on May 27th and we are fully booked for June and most of July, part of August. We can readily find additional surgical slots for families in need.
The following are some of the protocols put in place. I can assure you that our team and the entire Mount Sinai organization are and will do everything possible to prevent exposure to COVID-19. During office hours, there will only be one patient seen at a time, we will not have multiple patients in exam rooms at any given time. Patients and their families will be asked about symptoms of COVID and if they are symptomatic, they will be tested and not be seen. Only one parent can come in with the patient in order to minimize exposure for anyone. We can do FaceTime for a second parent who might want to be part of the discussion. I have done that frequently throughout my career. All patients and family members and staff will wear a mask at all times. The rooms and facilities are frequently being cleaned over and over and over again. Telemedicine or E-consults will remain a good option for all families before and after surgery but we will need to see preoperative patients at least one time prior to surgery.
All surgical patients will be tested at Mount Sinai within two days prior to surgery, only one parent will be allowed to stay at the hospital and with their child after surgery at a time. The parent will have to wear a mask throughout the hospital stay. The facilities have been cleaned, sterilized, inspected and are constantly being cleaned. Patients will not be roomed anywhere near a COVID + patient.
I can very much appreciate the families’ and patients’ concerns. Let me assure all that Mount Sinai Hospital is a world-class institution. I was personally involved in the care of COVID patients several weeks ago, the hospital teams have amongst the most experience with this disease than any other hospital in the United States. The protocols have been developed and refined with the highest level of expertise. I am proud to say, thousands of lives were saved at Mount Sinai Hospital during this pandemic. My patients and their families will, as always, be the highest priority of my team and I and the hospital staff are looking forward to welcoming and caring for them. We will be available 24-7 to ensure a safe and comfortable experience.
Stay well, be healthy, and let us all have a renewed appreciation for all the blessings we have in life.
My best to all,
Baron Lonner. M.D.
Chief of Minimally Invasive Scoliosis Surgery
Mount Sinai Hospital
Coronavirus Disease 2020 (COVID-19)
Dear Patient and Family,
Our Team at Scoliosis Associates and Mount Sinai Hospital Spine understand that you and your family may be experiencing personal hardships or concerns related to the COVID-19 Coronavirus outbreak and pandemic. We also understand that you would like your child or other family member to receive care, recommendations and counseling about their spinal condition.
My team and I are here for you, we will be available via email, Telemedicine and E-Consults and look forward to resuming standard practice as soon as this current event passes.
In the meantime, we ask that you reach out to us with any questions or to arrange an E-consult. Please reach out to Patricia Permaul, 212-241-8312, or by email, patricia.permaul@mountsinai.org. Future office visits in the weeks and months ahead can be arranged through our appointment line, 646-499-3715.
Stay well, my very best to you, your family, and friends,
Baron Lonner, MD
Chief of Minimally Invasive Scoliosis Surgery
Mount Sinai Hospital
Professor of Orthopaedic Surgery
Icahn School of Medicine
Mount Sinai Spine Center
5 East 98th St, 4th floor, Box 1188
New York, NY 10029
Office: 212-241-8312
Appointments: 646-499-3715
Fax: 646-537-9449
www.scoliosisassociates.com
Dr. Baron Lonner Presenting at Setting Scoliosis Straight Foundation
Dr. Baron Lonner Presenting at Setting Scoliosis Straight Foundation
Dr. Lonner is seen presenting at a research meeting of the Setting Scoliosis Straight Foundation. He serves on the Board of this organization which fosters research into the treatment of pediatric scoliosis and related spinal deformities. He has authored over 100 publications on spinal deformities based on clinical research that he and others designed to answer important questions for patients and their families. These studies have directly impacted Dr. Lonner’s surgical and non-operative treatment of patients and those of other surgeons and is what drives his passion for research- providing the best and safest possible care for patients.
Dr. Lonner Presents Research at Annual Scoliosis Research Society Meeting
Dr. Lonner Presents Research at Annual Scoliosis Research Society Meeting
The Scoliosis Research Society was founded in 1965 with a twofold mission: to educate surgeons and to facilitate optimal care of patients with scoliosis and other spinal deformities. The annual meeting of the Scoliosis Research Society brings together medical leaders from all over the globe with the overarching aim of the society in mind, providing researchers and medical practitioners with a forum to share new research and discuss important trends in order to improve the quality of treatment and care options for patients with spinal deformities. Our own Dr. Baron Lonner, MD, a top scoliosis spine surgeon and member of the Board of Directors of the SRS, spoke at this year’s annual meeting, which was held earlier this month in Minneapolis, Minnesota. Dr. Lonner is the chief of the Division of Spine Surgery Mount Sinai Beth Israel, as well as a leading professor of Orthopedic Surgery.
“The Scoliosis Research Society is comprised of leaders and practicing surgeons from around the world who gather every year to share current research and trends in the care of patients with scoliosis and spinal deformities,” Dr. Lonner explained. “This society has spread knowledge amongst surgeons around the world that has directly impacted hundreds of thousands of patients. Members of the SRS have become my friends and our collaborations together have furthered the well-being of patients, their treatment with surgical and non-surgical techniques, and led to improved and safer results or outcomes following surgery.”
Dr. Lonner was especially honored to be a part of this year’s annual meeting, as it was dedicated to commemorating advancements made in the care and treatment of those with spinal deformities. “This year’s meeting was special because it was a celebration of our collective history and the lessons we have learned in helping our patients,” Dr. Lonner said. “I was honored to have three podium presentations, including one in which I discussed the latest techniques in scoliosis and kyphosis care.” He also presented papers on decreasing blood loss in scoliosis surgery and operative treatment of Scheuermann kyphosis, a condition that increases the normal round back in the upper spine, resulting in a hunchback-like appearance.
Dr. Lonner and the SRS Board of Directors
Over the course of the past 50 years, the Scoliosis Research Society has positively impacted the lives of hundreds of thousands of patients. Dr. Lonner is proud to be a member of this society and to serve its overarching mission, having served on several of the organization’s taskforces. Dr. Lonner is a leading spine surgeon in the Mount Sinai Hospital and Health System and is the Chief of the Division of Spine Surgery at Mount Sinai Beth Israel. As an active researcher and having presented dozens of research papers in meetings around the world, Dr. Lonner hopes to continue making valuable advancements in the field of spinal deformities.